All of us have experienced the self-healing properties of the human body. Often times, a few bumps and bruises in our youth are simply part of life. The process of human growth and development involves complex cellular activity which fosters growth and tissue maturity. The availability of growth hormones and constant activity of bone and muscle cells allows the body to more readily repair tissue injury.
However, as we age there a far more barriers to healing. Still, the reality is that the human body has a vast potential for healing either by compensating for imbalances or adapting to tissue changes. Whether you injure muscle, cartilage, nerve or bone, the body has been designed to work toward restoring balance. This does not mean that the tissue will return to its original state. Instead, the nervous system will often trigger adaptations which allow one system (i.e myofascial chains) to compensate for a deficiency in another system (i.e joint cartilage).
An emerging medical practice is hoping to tilt the scales more in favor of healing. Regenerative medicine has demonstrated some potential benefits for specific conditions which are prone to delayed healing. Yet, it is important to keep in mind that a fix rarely exists in the human body since function relies upon the balance of the entire neuromusculoskeletal system. This is where physical therapy plays an important role for regenerative medicine.
Despite the body’s amazing ability to regenerate, external factors such as chronic inflammation, advanced age, or poor immune function may keep the body from fully healing. To counteract this, the discipline of regenerative medicine has been on the rise. Regenerative medicine refers to the branch of medicine that deals with “the process of replacing, engineering or regenerating human cells, tissues or organs to restore or establish normal function” [1]. The ultimate goal of regenerative medicine is to re-engineer damaged tissue by stimulating the body’s own repair mechanisms. How is this accomplished? One primary means is through cellular therapies. Cell therapy or cytotherapy works by injecting cellular material to targeted systems or areas of injury. Through the influx of cellular material, the damaged tissue has an increase of nutrition that it needs in order to regenerate.
One particular field of interest is the introduction of stem cells to enhance the healing potential of injured tissue. Stem cells are unique in that they are not specialized cell types, but instead have the ability to transform into whatever tissue they contact; whether it be muscle, bone, ligament, or tendon. Moreover, stem cells undergo numerous cell division cycles allowing for regeneration to occur at a natural rate as compared to older tissue which replenishes at a slower rate. Recent research has shown promise that stem cells may be the future of recovery after spinal cord injury or in the effort to “regrow” meniscal cartilage in the knee.
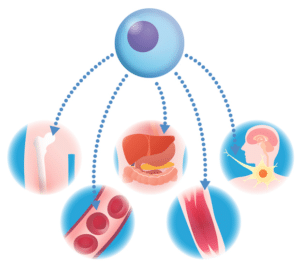
Figure 2. Stem cells can generate to a variety of body tissue.
As new treatments are being developed, physical therapy should not be ignored.
A recent animal study demonstrated that early mobilization after injection of extracellular material to damaged achilles tendons played a critical role in tendon remodeling as well as tendon regeneration through circulating growth factors [2]. Additional research has suggested that the application of therapeutic exercise increases the activity of stem cells as well as helps recruit donor cells to the site of interest [3, 4]. It appears that exercise is a beneficial means to stimulate the regeneration of tissue after stem cells have been injected. Therefore regenerative medicine is incomplete without participation in a therapeutic program which involves skilled mobilization and exercise.
Understanding Tissue Healing Timeline
Having an awareness of tissue healing timeline is the key to the rehabilitation process. According to Clanton et al, there are 5 phases of tissue healing.
- PHASE 1: Acute phase: (1 to 7 days)
- PHASE 2: Subacute phase: (Day 3 to < 3 weeks)
- PHASE 3: Remodeling phase: (1 to 6 weeks)
- PHASE 4: Functional phase: (2 weeks to 6 months)
- PHASE 5: Return to competition phase: (3 weeks to 6 months)
Regardless of tissue, the body goes through a linear progression of healing until the body is whole. The higher vascularity of tissue, the quicker the progression is through the healing timeline. For example, a strained muscle may fully heal in as little as 6 weeks because of its increased blood flow whereas a fractured bone will take close to 6 months due to its poor vascularity.
Regenerative medicine is indicated for certain conditions when the body becomes stuck in PHASE 3: Remodeling Phase. Due to a wide variety of factors, specific tissue may not have the complete cellular material matrix required to fully remodel. The application of stem cells in combination with physical therapy may be the answer to completing the remodeling phase.
Regenerative Medicine and Northern Edge Physical Therapy
At Northern Edge Physical Therapy we understand the emerging relationship between regenerative medicine and physical therapy. Regenerative medicine is unique per client and unique per tissue. At Northern Edge, we address tendon and ligament regeneration through low load progressive exercise (LLPE).
The fiber orientation of tendon and ligaments respond to progressive loads. The combination of eccentric loading with minimal impact is crucial for properly loading tendon and ligament tissue. Our primary means for accomplishing this is through the revolutionary Redcord system and anti-gravity Alter G treadmill. In regards to osseaous tissue (bone) regeneration we respect Wolf’s Law and advance the exercises to include graded loading for bone hardening and remodeling. We use advanced technology like force plates, instrumented treadmill, EMG and high speed infrared cameras to analyze the motion, force and alignment of joints as our clients progress towards full activity or return to sport.
Finally for nerve tissue regeneration, our program includes aerobic based training for increased tissue nutrition as well as nerve flossing techniques to ensure pliability of the nervous system.
Regenerative medicine is a new and exciting topic in the field of medicine. As advancements with cellular therapies are discovered, it is important to keep in mind the conservative measures and benefits of low load progressive exercise.
Research:
[1] Regenerative Medicine, 2008, 3(1), 1–5 [47].
[2] Hodde JPB, Bradylak SF, Shelbourne KD. The effect of range of motion on remodeling of small intestinal submucosa (SIS) when used as an Achilles tendon repair material in the rabbit. Tissue Eng. 1997;3:27-37.
[3] Palermo AT, Labarge MA, Doyonnas R, et al. Bone marrow contribution to skeletal muscle: a physiological response to stress. Dev Biol. 2005;279:336–344.
[4] Bouchentouf M, Benabdallah BF, Mills P, Tremblay JP. Exercise improves the success of myoblast transplantation in mdx mice. Neuromuscul Disord. 2006;16:518–529.
[5] Arnheim DD. (1995) Essentials of athletic training. St Louis: CV Mosby Co.

0 Comments